Introduction
 Low back pain is one of the most common causes of disability and affects up to 80% of the population at some time during their active life. The Oswestry Disability Index (ODI) is the most commonly used outcome measure to help measure for pain and disability resulting from low back pain.
Low back pain is one of the most common causes of disability and affects up to 80% of the population at some time during their active life. The Oswestry Disability Index (ODI) is the most commonly used outcome measure to help measure for pain and disability resulting from low back pain.
First published in 1980 and revised in 2000, the ODI has been widely used as a condition-specific outcome measure for patients with spinal disorders, and was developed for use in secondary care settings.
The ODI is considered by many as the benchmark for measuring degree of disability and estimating quality of life in a person with low back pain.
“The ODI remains a valid and vigorous measure and has been a worthwhile outcome measure.”
Spine Volume 25 – Issue 22
Mode of Use
 The ODI is a self-administered questionnaire divided into ten sections designed to assess limitations of various activities of daily living and reflecting the patient’s ability to manage their everyday life while dealing with their pain. The items include:
The ODI is a self-administered questionnaire divided into ten sections designed to assess limitations of various activities of daily living and reflecting the patient’s ability to manage their everyday life while dealing with their pain. The items include:
- Pain intensity
- Personal care (e.g. washing and dressing)
- Lifting
- Walking
- Sitting
- Standing
- Sleeping
- Sex life (if applicable)
- Social life
- Traveling
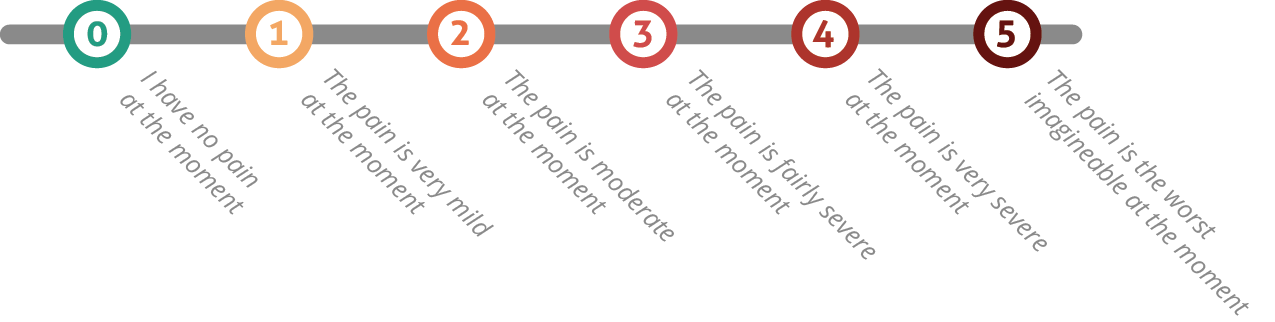
Each topic category is followed by 6 statements describing different potential scenarios in the patient’s life relating to the topic. The patient then checks the statement which most closely resembles their situation. Each question is scored on a scale of 0-5 with the first statement being zero and indicating the least amount of disability and the last statement is scored 5 indicating most severe disability.
The patient is asked to complete the ODI and answer based on the statement they feel applies to them. In clinical settings, it can be used at baseline and at intervals thereafter while treatment continues.
The questionnaire takes 3.5–5 min to complete and approximately 1 min to score. It has been delivered in many formats, including paper, telephone, SMS, and web-based.
Scoring and Interpretation
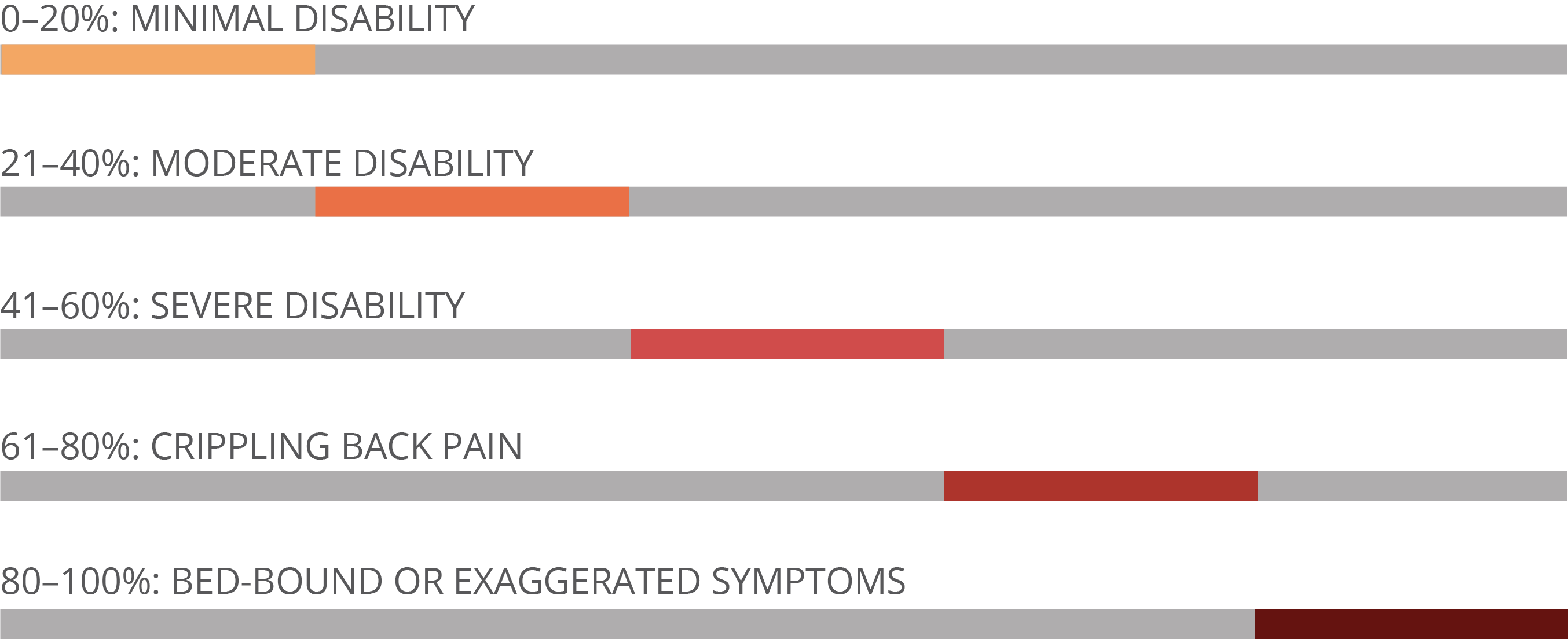
Each of the ten items in the ODI has six statements from which patients are requested to select one. This allows scoring from 0-5 for each item, for example, looking at the first item.
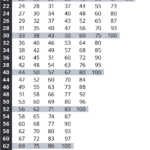
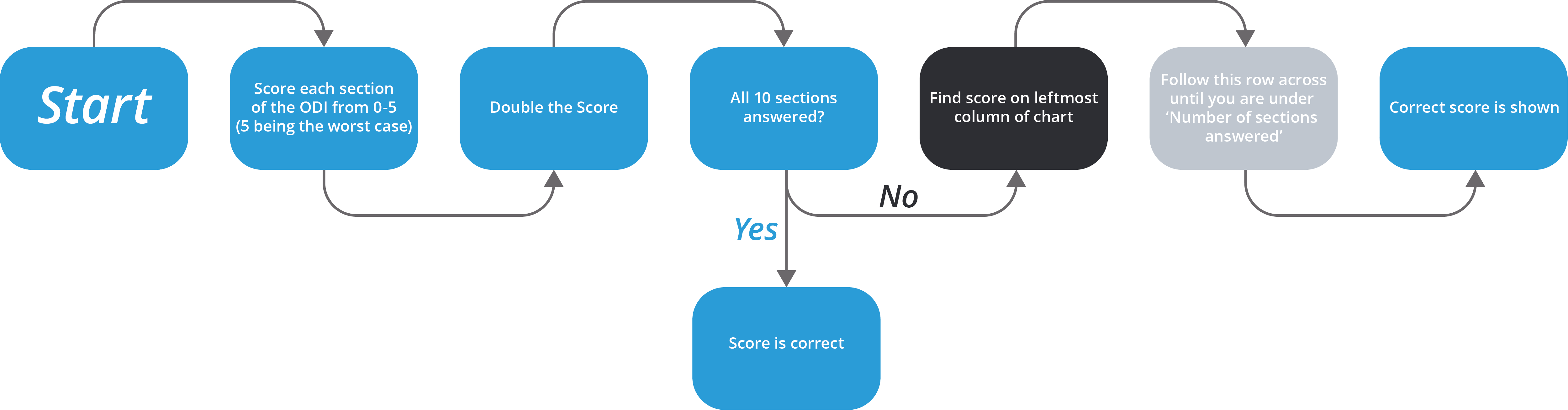 Questions not answered are not counted towards the total. With ODI questionnaires where one or more sections are unanswered, the correct score should be calculated by reducing the denominator by 5 for every unanswered section.
Questions not answered are not counted towards the total. With ODI questionnaires where one or more sections are unanswered, the correct score should be calculated by reducing the denominator by 5 for every unanswered section.
A handy table has been created to aid in scoring incomplete questionnaires, and can be posted where scoring is done.
Translations
The ODI questionnaire has been translated into dozens of languages, with many of these translations carried out by Mapi’s team of language experts. To find out more, please visit ePROVIDE™
Author

Jeremy Fairbank was educated and trained at Cambridge University and St Thomas’ Hospital. He qualified MB.BChir from Cambridge University in 1972 and became a fellow of the Royal College of Surgeons of England (FRCS) in 1977. He obtained an M.D. for a thesis on the facet joint in back pain in 1982 awarded by Cambridge University.
Jeremy’s training included two years as a Spinal Fellow in the Robert Jones and Agnes Hunt Orthopaedic Hospital in Oswestry (1998) where he published the Oswestry Disability Index which has become a worldwide standard for assessing back pain and the results of treatment. This was followed by four years as a Senior Registrar in the St Bartholomew’s Hospital Training Programme. In 1984 he was appointed Consultant Trauma and Orthopaedic Surgeon to the General Hospital and Royal Orthopaedic Hospital in Birmingham, and in 1989 he moved to Oxford.
Professor Fairbank is currently employed by the Oxford University Hospitals as Consultant Orthopaedic Surgeon with a special interest in spinal disorders. The vast majority of his work is devoted to treatment of disorders of spine, including fractures, tumours, infections, spinal deformities (scoliosis and kyphosis) and back pain. Jeremy has been a Professor of Spinal Surgery since 2006.
References
- Wikipedia entry on the ODI
- Fairbank JC, Couper J, Davies JB. The Oswestry Low Back Pain Questionnaire. Physiotherapy 1980; 66: 271-273.
- Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine 2000 Nov 15;25(22):2940-52
- National Council for Osteopathic Research’s overview of the ODI
- Baker DJ, Pynsent PB, Fairbank JCT. The Oswestry Disability Index revisited: its reliability, repeatability and validity, and a comparison with the St Thomas Disability Index. M. Roland, J.R. Jenner (Eds.), Back pain: new approaches to rehabilitation and education, Manchester University Press, Manchester (1989), pp. 174–186
- Davidson M, Keating JL. A comparison of five low back disability questionnaires: reliability and responsiveness. Physical Therapy 2002;82(1):8–24
- Laurdisen HH, Hartvigsen J, Manniche C, et al. Danish version of the Oswestry Disability Index for patients with low back pain. Part 1: Cross-cultural adaptation, reliability and validity in two different populations. European Spine Journal. 2006;15(11):1705-16.
- Mannion AF, Junge A, Fairbank JC, et al. Development of a German version of the Oswestry Disability Index. Part 1: cross-cultural adaptation, reliability, and validity. European Spine Journal. 2006;15(1):55-65.
- Pynsent PB, Webb M. Management of low back pain in Primary Care. Oxford: Butterworth Heinemann; 2001. The prevalence of low back pain in Great Britain; pp. 19–25.
- Palmer KT, Walsh K, Bendall H, Cooper C, Coggon D. Back pain in Britain: comparison of two prevalence surveys at an interval of 10 years. BMJ. 2000;320:1577–8.
- Waddell G. The epidemiology of low back pain. In: Waddell G, editor. The Back Pain Revolution. Edinburgh: Churchill Livingstone; 1998.
Roland M, Morris R. A study of natural history of back pain. Part I: Development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8:141–4. [PubMed] - Roland M, Morris R. A study of the natural history of back pain. Part II: Development of guidelines for trials of treatment in primary care. Spine. 1983;8:145–50.
- Waddell G, Main CJ. Assessment of severity in low-back disorders. Spine. 1984;9:204–8.
- Million R, Hall W, Nilson KH, Baker RD, Jayson MIV. Assessment of the progress of the back pain patient. Spine. 1982;7:204–12.
Contact Us
Please contact our PROVIDE™ team for any questions on the ODI:
Mapi Research Trust
PROVIDE™
27 rue de la Villette
69003 Lyon
France
Telephone: +33 (0)4 72 13 65 75


